Full and Partial knee replacement surgery for chronic knee pain
“Degenerative joint disease (arthritis) is not a life-threatening disorder; it is a functional disability.”
~ Prof Lo Ngai Nung
Knee replacement surgery should be considered only if this is the last measure for your knee pain. This article based on an interview with Prof. Lo Ngai Nung, Consultant Orthopaedic Surgeon at the Orthopaedic Specialist Practice. He explains knee pain in elderly patients and the options to live pain-free.
The knee joins the thigh bone (femur) to the shin bone (tibia). The smaller bone that runs alongside the tibia (fibula) and the kneecap (patella) are the other bones that make the knee joint. Tendons connect the knee bones to the leg muscles that move the knee joint.
The knee joint takes a lot of loads to allow us to stand, walk and run. It also has to be flexible and stable to allow us to bend, squat and dance and take on heavy loads.
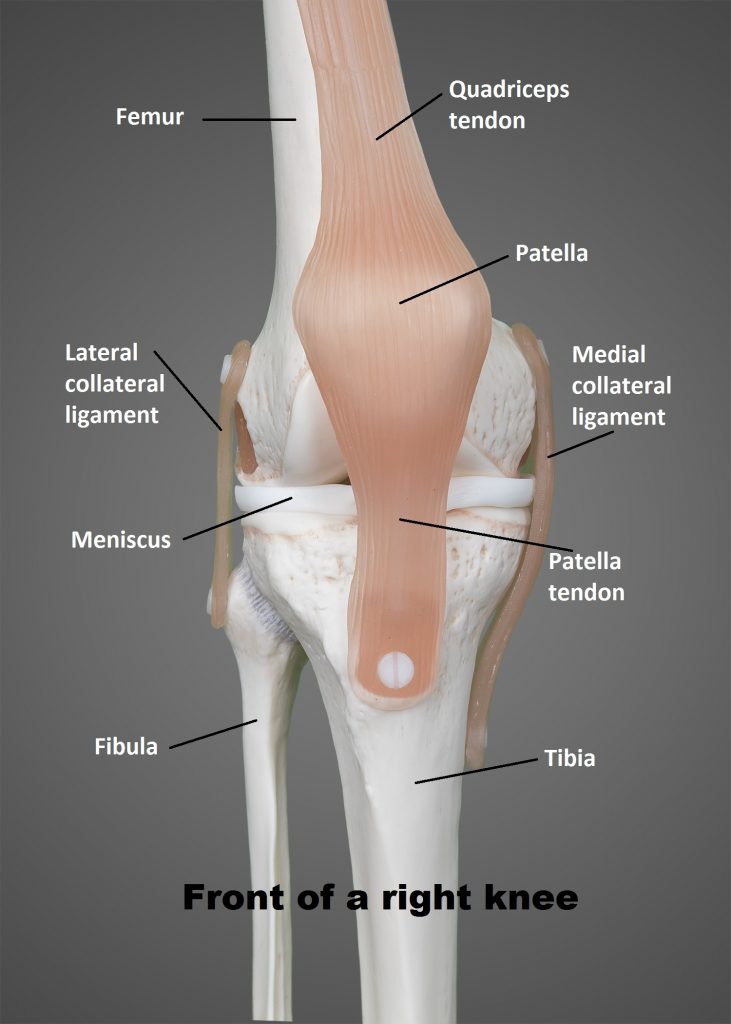
Knee Anatomy Model
Parts of the knee:
- Tendons connect the knee bones to the leg muscles that move the knee joint.
- Ligaments join the knee bones and provide stability to the knee
- cartilage called the medial and lateral menisci act as shock absorbers between the femur and tibia.
- fluid-filled sacs, help the knee move smoothly.
It is common in elderly patients to experience pain in the knees from overloading or activity.
Seek doctor’s advice when:
- Aches and pains are persistent or reoccurring over a period of time
- associated with recurring swelling or inflammation
- Stiffness and locking in the knee (mechanical derangements and jamming)
- Deformity – walking unstable or wobbling
- Affect daily function
Factors that can be adjusted to lower risk of wear and tear of the knee joint:
- Bodyweight
- Muscle strength
- Reduce high impact activities
- Choosing the right sports activities when one is already prone to knee injuries
Visit an orthopaedic surgeon for an opinion or treatment plan:
- Detailed history taking
- Background of pain
- Duration of pain
- Cause of pain
- Treatments patients have undergone
- Detailed analysis if knee trouble affecting daily life
- Response to alternative treatments
- Clinical examination of the patient
- Is the pain coming from the knee?
- Is the joint stiff?
- Is there swelling in the joint?
- Is there a malalignment or a discrepancy problem?
- Other factors to consider:
- Overweight issue
- Muscle weakness
- Spine or hip problem
- Investigation
- X-ray of patient’s joints
Non-surgical options are primarily advised by the doctor. They include:
- Losing weight
- Strengthening of muscles
- Physiotherapy – exercise therapy
- Walking aid – walking stick
- Managing symptoms through pain medication – topical medication, oral medication, injections
Surgery should be considered:
- When alternative treatments and life adjustments made don’t relieve pain
- Good health
- Risk issues
- Get back to a pain-free knee
Man-made implant – Full knee replacement
- Replace the damaged surfaces with a metal-plastic implant
- About 8-9mm thick
- Its shapes are a curvature similar to a natural knee surface
- Covers the damaged cartilage surface with a smooth polish metal cap
- Below is a plastic tray sitting on a titanium platform that takes place of the damaged cartilage or damaged meniscus on top of the tibia
When a patient comes in earlier stages of their condition damage is localized, in the instances of a torn cartilage meniscus on one side, then a partial knee replacement can be considered.
The surgery
- Day 1: Surgery duration of 1.5 hours
- Day 2: Physiotherapy to strengthen muscles and improve balance
- Day 3: Patient walks down the corridor and learns to climb stairs. When a patient is confident to get out of bed themselves, sit and stand, go to the bathroom themselves, holding on to a walking stick, then patients go home.
- Day 6: Follow up check-up on their exercises and walking ability and no other complications such as swelling
- 2-3 months: the patient should spend some effort working on muscle strength, regaining joint flexibility, and balance
Making an appointment
To make an appointment with Prof Lo Ngai Nung, his contact details are
- web: www.ospr.com.sg
- phone: +65 6265 2388
- Whatsapp: +65 831 86243
For Physioactive Singapore, find your closest location at www.physioactive.sg
For Physioactive Indonesia, book directly online click here.